Photodynamic Therapy (PDT)
-- Non-invasive option for many skin conditions
Photodynamic therapy (PDT) is a medical treatment that utilizes a special “photosensitizing drug” (that becomes activated by light exposure) and a light source to activate the administered drug. PDT is a non-invasive treatment modality for solar precancerous skin damage (actinic keratoses) and some early superficial forms of skin cancers, including superficial basal cell cancer, and in-situ (intraepidermal) squamous cell cancer. It is an evidence-based alternative to cryotherapy, surgery and superficial radiation therapy for these forms of non-melanoma skin cancer.
Acne, rosacea, sun damage, enlarged sebaceous glands, wrinkles, warts, hidradenitis suppurativa, psoriasis, and many other skin conditions can also be treated effectively with PDT, resulting in long periods of clear skin.
The procedure is easily performed in a doctor’s clinic as an outpatient. This treatment works well and has few long-term side effects.
PDT essentially has three steps. First, a light-sensitizing liquid or cream (photosensitizer) is applied to the targeted treatment area. Occasionally, a photosensitizing molecule that is already part of the body can be activated. Second, there is an incubation period of minutes to days (usually the incubation time is just over an hour long). Finally, the target tissue is then exposed to a specific wavelength of light that then activates the photosensitizing medication. The most frequently used frequencies are blue (415nm) and red (633 nm). The mechanism by which tissue is destroyed seems to depend on the presence of activated oxygen molecules.
Steps:
- application of photosensitizer drug (most commonly applied as a cream containing 5–aminolevulinic acid [5–ALA] or methyl aminolevulinate [Metvix®])
- incubation period (usually just over an hour)
- light activation (blue or red light frequencies)


PDT for Acne
PDT can be a very effective treatment option for some forms of acne and may lead to long periods with almost complete acne clearance, without the potential side effects of antibiotics and isotretinoin (Oratane, Accutane, Roaccutane). It is indicated for moderate forms of acne with inflammatory lesions (red with small pustules), and a series of treatment sessions is suggested.
It is important to be aware that the first 1-2 sessions may cause a temporary flare-up for a few days, yet the resulting improvement in acne is fairly rapid for most patients. Often the results are long-lasting, and extra sessions can be scheduled a few months later if needed.
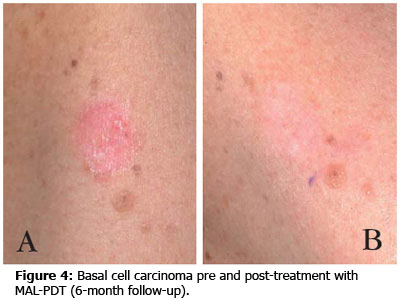
PDT for early skin cancers
Superficial Basal Cell carcinomas and Squamous Cell Carcinoma in-situ (IEC or Bowen’s disease) can be treated very effectively using PDT. A biopsy (or results from a previous biopsy) is required to confirm the cancer is only superficial (deeper cancers do not respond adequately to the treatment and usually require surgery). The expected complete response rate is up to 97% after 12 months, and 81.8% after four years follow-up, which compares with 95% long term cure rates with surgery.

Photodynamic Therapy FAQ
What are the benefits of PDT therapy?
How does PDT work?
What does the PDT treatment involve?
Our doctor’s experience and knowledge guarantees that only appropriate lesions are treated.
What to expect after the treatment?
Generally healing is complete within seven to ten days. You are advised not to have any sunlight exposure for four days after the treatment and avoid applying makeup until the area has settled.
What follow-up is required after PDT treatment?
How much improvement can I expect with PDT?
No two people are the same, and results may vary. Some conditions can improve dramatically in some patients and not respond in others.
Overall, patients with severely sun-damaged skin with actinic keratosis, mottled pigmentation, dull or sallow skin, and skin laxity, may see good to excellent improvement with PDT. There can be improvement of large pores, non-pitted acne scars, and active acne.
Depending on the area being treated and the recommended incubation time, different numbers of treatment sessions spaced 4 to 6 weeks apart may be required to achieve the desired improvement and reduction in lesions. On average, one treatment is sufficient for sun-damaged skin and actinic keratosis, yet for acne and skin cancers a series of two to three treatments may be needed. It is not always possible to predict ahead of time how many treatments your specific condition may take or how you will respond to PDT.
After photodynamic sun avoidance for 24-48 hours is necessary.
What is the cost of PDT treatment?
The treatment cost is between $350 and $500 depending on the size of the area treated. A further Medicare rebate of $75 may apply. If you have a health care fund you may be able to claim part of the cost of the treatment (related to the photosensitizer medication used). We recommend inquiring with your health care fund prior to the treatment day.
What adverse reactions can occur with PDT?
Some redness, swelling and crusting is expected after the procedure but generally will resolve within a few days. Redness, weeping and crusting will develop after treatment and will need simple bathing and dressings. Occasionally, more severe swelling, blistering, weeping or itching may occur. In some cases the skin may become lighter or darker in colour. Increased skin colour generally fades over months but decreased skin colour can occasionally be permanent.
Serious side effects are very rare, but may include: anxiety (during the procedure), headaches, dizziness, and skin infections.
When is PDT not used?
People with a strong sensitivity to light or with photosensitive disorders such as lupus, may not be appropriate candidates for this form of treatment. People who suffer from anxiety or claustrophobia may find the dressings and close application of strong light difficult to bear.














